 High food pesticides found in children with type-1 diabetes
High food pesticides found in children with type-1 diabetes
SOURCE: Journal of Clinical Toxicology, Vol. 2(6): 2012
Mansoura University Children's Hospital, Egypt
Department of Toxicology & Food Contaminants
Does eating conventional grocery store food grown with chemical pesticides increase the risk for developing type-1 diabetes?
This was one of several questions researchers wanted to answer at Mansoura University Children's Hospital in Egypt. The basic premise of the study was that if pesticide residues in food did increase diabetes - we would then see higher levels of these pesticides in children with type-1 diabetes.
 STUDY DESIGN: The study was started with 75 children under age ten who were diagnosed with type-1 diabetes within the past 30 days. Blood samples were taken from all children and also from 35 healthy control children who did not have diabetes. Blood samples in both groups were then tested for nine different pesticides. This included the pesticide lindane (used in head lice treatments and also in food crop agriculture), the agricultural pesticides malathion, chlorpyrifos and profenofos and also the pesticides DDT and DDE. While most people assume DDT is no longer used, this is actually incorrect as some countries in Africa and South America still use DDT in agriculture, and these foods are frequently imported into Europe and the United States, especially during the winter months. Another source of DDT in foods comes from a little publicized fact that the common pesticide dicofol (routinely used on citrus) contains DDT as an unintended by-product during manufacture.
STUDY DESIGN: The study was started with 75 children under age ten who were diagnosed with type-1 diabetes within the past 30 days. Blood samples were taken from all children and also from 35 healthy control children who did not have diabetes. Blood samples in both groups were then tested for nine different pesticides. This included the pesticide lindane (used in head lice treatments and also in food crop agriculture), the agricultural pesticides malathion, chlorpyrifos and profenofos and also the pesticides DDT and DDE. While most people assume DDT is no longer used, this is actually incorrect as some countries in Africa and South America still use DDT in agriculture, and these foods are frequently imported into Europe and the United States, especially during the winter months. Another source of DDT in foods comes from a little publicized fact that the common pesticide dicofol (routinely used on citrus) contains DDT as an unintended by-product during manufacture.
 EVIDENCE OF A LINK: By comparing pesticide levels in children with and without diabetes, doctors could easily see if a pattern exists. For example, if pesticide levels were higher in children with diabetes, it strongly suggests that eating conventionally grown foods over the years is contributing to autoimmunity and increasing rates of type-1 diabetes. If levels were the same in both groups it would suggest consuming pesticide residues in food was not a problem.
EVIDENCE OF A LINK: By comparing pesticide levels in children with and without diabetes, doctors could easily see if a pattern exists. For example, if pesticide levels were higher in children with diabetes, it strongly suggests that eating conventionally grown foods over the years is contributing to autoimmunity and increasing rates of type-1 diabetes. If levels were the same in both groups it would suggest consuming pesticide residues in food was not a problem.
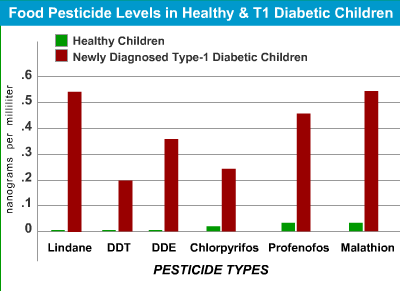
Below are results from both groups of children. As can be seen by the higher numbers in diabetic children - eating foods grown using conventional pesticide agriculture would appear to play a significant role in the development of type-1 diabetes. In fact, children with type-1 diabetes were found to have a remarkable 10, 20 and even 50 times higher level of pesticides in their blood than children without diabetes. Each row shows the pesticide type and levels found in healthy and diabetic children. Measurements in nanograms per milliliter of blood (ng/ml).
| Pesticide Type |
Healthy Children |
Diabetic Children |
Amount Higher |
| Lindane | Not Detectable | .54 | >54x higher |
| DDT | Not Detectable | .20 | >20x higher |
| DDE | Not Detectable | .37 | >37x higher |
| Chlorpyrifos | .02 | .24 | 12x higher |
| Profenofos | .03 | .46 | >15x higher |
| Malathion | .03 | .54 | 18x higher |
| TOTAL BURDEN | .08 | 2.35 | 29x higher |
In looking at the chart, we see the following:
1. Healthy non-diabetic children had no mesurable levels of the pesticide lindane (top row) -
but children with diabetes had a level of 0.54.
2. Healthy children had no measurable levels of the pesticide DDT (second row) -
but children with diabetes had levels of 0.20.
3. Healthy children had no measurable levels of the pesticide DDE (third row) -
but children with diabetes had levels of 0.37 .
The same pattern was seen with the common organophosphate pesticides chlorpyrifos, profenofos and malathion.
Chlorpyrifos levels were averaging .02 in the healthy children,
and .24 in children with diabetes.
The moderate to severely toxic pesticide profenofos was .03 in healthy children,
but
15x higher in diabetic children with levels of .46.
The same pattern was also seen for the pesticide malathion. Healthy non-diabetic children had malathion levels of .03, but children with type-1 diabetes had malathion levels 18 times higher at .54.
When using these numbers to determine increased risk from the pesticides, the researchers found that children with the higher levels of malathion had a 4 times greater risk of developing diabetes than children with low levels of malathion.
What is very worrisome, when looking at the total body burden of pesticides in diabetic children compared to non-diabetic children, the total difference was immense - While healthy children had a total blood pesticide level of .08 (all pesticides together) - children with newly diagnosed diabetes had an average total level 29 times higher at 2.35. To put this into context, this means that children recently diagnosed with type-1 diabetes had 29 times more of these poisons traveling through their blood every minute and to all cells and organs in their body than children without diabetes.
HOW FOOD PESTICIDES INCREASE DIABETES
In other parts of our report at gdrp.me, we've provided detailed documentation on how pesticides can damage parts of the human body that protect us from autoimmunity. This includes the organ called the thymus, as well as our immune system's natural killer cells - which make up about 5% of our total white blood cells and (when working properly), can release substances that quickly calm any ongoing autoimmune attack.
Along with this, many pesticides (including those found in this study) are listed as endocrine disrupting chemicals. This means they have the potential to increase glucose levels by contributing to insulin resistance. Interestingly, many children with type-1 diabetes are now being been found to have signs of insulin resistance - which is the hallmark of type-2 diabetes. So, instead of only type-1, diabetic children are now being called type 1.5 (a combination of both type-1 and type-2).
THE SMOKING GUN:
EVIDENCE FOR "CAUSE" AND "CAUSING" DIABETES
Since children with diabetes have higher blood levels of pesticides used in food agriculture (when compared to children without diabetes) - it strongly suggests these chemicals play a role in making diabetes appear earlier than it would otherwise. It must be considered that exposing a child to food pesticides day after day could increase autoimmunity through any of a number of different mechanisms. Since the pancreas has been shown to regenerate beta-cells continuously in both children and adults, this would also suggest that daily exposure to pesticides in food could prevent some or all children from reaching a partial-remission (honeymoon) and may even prevent full remission. Testing this hypothesis would be easy to do for anyone with a child with diabetes by simply putting their child on an organic diet for 2-3 weeks and monitoring morning fasting blood sugar.
WHY SOME CHILDREN HAVE HIGHER PESTICIDES?
One very important question is why do children with diabetes have so much more pesticides in their bodies than children without diabetes. Below are several situations and biological conditions that could explain this:
| 1. | Eating Foods with High Pesticide Residues Some foods are well known for having higher levels of pesticides compared to others. If a child eats more of these foods, he/she would be expected to have higher blood levels of these pesticides. The Environmental Working Group has identified the foods with the highest pesticide levels. The eight most contaminated are: strawberries, spinach, nectarines, apples, peaches, pears, cherries and grapes. It's not just veggies, according to the EPA, meat is contaminated with higher levels of pesticides than any plant food. Many chemical pesticides are fat-soluble and accumulate in the fatty tissue of animals. Animal feed often contains animal products (bone & blood) which adds even more pesticide problems, which is then directly passed to the human consumer when eating meat. |
| 2. | Weight Loss Many pesticides are stored in fat. When someone begins to lose weight, fat is burned for energy. This in turn, releases all the pesticides stored in the fat over the years. If a diagnosis of diabetes appeared even months after significant weight loss, it's reasonable to assume that the greatly increased blood levels of pesticides in their blood contributed to autoimmunity and the appearance of diabetes. |
| 3. | Weak Liver Enzymes The human liver is constantly working to break-down chemicals and pesticides into a "less toxic" form by a group of enzymes known as cytochrome P-450. Some people have been found to have one-third lower levels of these important enzymes. If this was the case with a child, any pesticides eaten in food would remain in their body for longer periods of time, thereby having more time to build to higher levels and cause greater amounts of damage inside the body. For those children with weaker liver enzymes - it is even more critical to reduce pesticide exposure in food. |
| 4. | Less Protection from Free Radical Damage You've probably heard of free radicals before. These are the bulls in the china shop inside every cell that play a role in aging and are formed as a by-product of basic oxygen metabolism inside the cell. Along with metabolism, free radicals are also formed after exposure to x-rays and many toxic chemicals including pesticides. Fortunately, there are mechanisms inside our cells that scavenge these free radicals and prevent them from doing too much harm. What is interesting is that children with diabetes have recently been found to have lower than normal level of natural anti-oxidant protection against free-radicals. Therefore, in this situation, free radicals would be expected to cause more harm in children with diabetes. Along with this, a number of scientific studies have shown that organic food has greater amounts of these free radical scavenging anti-oxidants (thereby, potentially making-up for some of the inherent weaker protection that may be present in a child with diabetes). |
HOW THE BODY REGENERATES NEW BETA-CELLS IN THE PANCREAS
Since the ability of the pancreas to regenerate new beta-cells is no longer theory and well documented to occur in both children and adults, it would be helpful to identify what takes place inside the body that encourages new beta-cell growth. Scientists at the Joslin Research Laboratories in Boston, Massachusetts were able identify one of these important processes. What they found was that all of us have a network of specialized cells located in the lining of our intestine where we digest food. These cells have the unique ability to produce what might be defined as a "magical" hormone called "exendin-4." The reason for the word "magical" is that when this hormone is produced by the cells in our intestine and enters the blood - it works as a powerful signal - telling specific parts of the pancreas to begin growing "new" beta-cells. These new beta-cells then grow from special areas within the pancreas known as progenitor ducts and can also grow from remaining beta-cells in the pancreas. Other research has shown alpha-cells in the pancreas (the ones that prevent low blood sugar) can literally transform into beta-cells if needed.
When this new beta-cell growth process starts at the suggestion of the hormone exendin-4, the body is attempting to replace beta-cells that have been destroyed by autoimmunity. You could almost say there is an ongoing race between one team trying to destroy beta-cells and the another team trying to build beta-cells. Unfortunately for children with type-1 diabetes, the team destroying beta-calls is winning, although exendin-4 is trying its best to help the "building team" turn this around.
This study can be seen in the journal Diabetes - Vol. 48(12): 2270-2276, Dec 1999
In another study outlined below, researchers showed a dramatic drop in blood pesticide levels in children just 2 days after switching to organic food. Along with this - we have been involved in a study with a middle-school student here in North Carolina who has had type-1 diabetes for nearly 3 years who showed dramatic improvements in c-peptide and fasting glucose after intense avoidance of phthalates, bisphenol-A and switching to an organic food diet. After suspending the organic diet at the end of 6 weeks, his improvements were erased and insulin requirements increased dramatically. For more information on the Gordon Diabetes Reversal Project please go to gdrp.me
THE NEXT STEP
With the information learned from the two studies on this page, the next step is to investigate if a 100% organic diet could improve diabetes - increase insulin output (c-peptide) - and reduce the amount of insulin children take at each meal. If improvements are consistently validated, insurance companies could be pursuaded to cover the cost of organic food, since it would be a medical intervention and save hundreds or thousands of dollars per month in insulin costs.
As evidence does suggest that pesticides may be increasing autoimmunity, it would also be informative to conduct a study to determine if switching to an organic diet could lead to lower autoantibody levels in siblings of children with diabetes, thereby reducing the risk of future type-1 diabetes.
Eating Organic Food Lowers Blood Pesticides in Children
SOURCE: Environmental Health Perspectives, Vol. 114(2): 260-263, Feb 2006
View Journal Online
In Children eating organic food (foods grown without pesticides) were found to have dramatically lower levels of pesticides when compared to eating conventional pesticide grown foods.
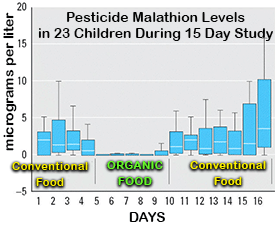 In this study, conducted in part by the Centers for Disease Control, scientists studied the effects of eating organic (non-pesticide) food among 23 elementary school children ages 3 to 11. Each child was tested daily for pesticide levels over 15 consecutive days. During the first 5 days (called phase 1) - children consumed their typical (pesticide) food diets. During phase 2 (days 6 to 10) - children ate only organic foods. In phase 3 (days 11 to 15), all children switched back to eating conventional foods grown with pesticides.
In this study, conducted in part by the Centers for Disease Control, scientists studied the effects of eating organic (non-pesticide) food among 23 elementary school children ages 3 to 11. Each child was tested daily for pesticide levels over 15 consecutive days. During the first 5 days (called phase 1) - children consumed their typical (pesticide) food diets. During phase 2 (days 6 to 10) - children ate only organic foods. In phase 3 (days 11 to 15), all children switched back to eating conventional foods grown with pesticides.
RESULTS: During phase 2, while eating organic foods, all children showed a dramatic drop in pesticide levels of chlorpyrifos and malathion (see chart above). Average levels of malathion metabolites while eating conventional food was approximately 1.2 micrograms per liter (of urine) but after switching to organic foods dropped to about less then 0.1 micrograms/liter. This represents a 12-fold decrease in body pesticide levels going from pesticide grown foods to organic foods. For the pesticide chlorpyrifos, (which has been linked to many health disorders affecting the brain and weakening the immune system), levels were approximately 6 micrograms/liter before eating organic and then dropped to 2 micrograms per liter while eating organic (a 3-fold reduction). Both malthion and chlorpyrifos are used extensively in agriculture with chlropyrifos also being used in home pest and termite control prior to 2002.
In conclusion, the researchers stated,
We were able to demonstrate that an organic diet provides a dramatic and immediate protective effect against exposures to organophosphorus pesticides that are commonly used in agricultural production....The persistent existence of OP pesticide metabolites in urine during the conventional diet periods raises a concern of the possible chronic exposures to OP pesticides in children.
Rollins School of Public Health, Emory University, Atlanta, Georgia, USA
University of Washington, Seattle, Washington, USA
Centers for Disease Control and Prevention, Atlanta, Georgia, USA
CHEM-TOX COMMENT: It is important that people realize that so-called safe levels of exposure are based upon studies done on "adults." Children have far lower levels of important liver enzymes that remove pesticides from the blood (i.e. paraoxanase) and this level can vary dramatically from one child to the next.. Therefore, chidren have pesticides remain in their blood for longer periods and at higher levels than adults. Also, critics of this study (such as those funded by agricultural interests) do not take into account that EPA guidelines on pesticide safety consider only at one pesticide at a time, however, children (and all of us) are exposed to many pesticides in food simulneously. This has been shown to result in far more harm than one pesticide alone, and can sometimes result in an exponential effect (1+1=100). Also, current EPA pesticide safety guidelines do not consider what is called subtle neurotoxicity (effects on learning/behavior) - subtle immune system effects (increased autoimmunity - lowering of white blood count - natural killer cell effects, etc.). The bottom line is that pesticides are designed specifically to kill - and our children are being exposed to small levels of these continuously in food. A follow-up study now needs to be done to determine if natural killer cells and autoimmunity are affected by these levels of pesticides.
Pesticides in Food - Diabetes Link
SOURCE: Indian Pediatrics, Volume 48:74, 2011
View Journal Online
 Below is the "Abstract" from the listed journal describing a patient who became ill after eating several non-washed tomatoe from a s:
Below is the "Abstract" from the listed journal describing a patient who became ill after eating several non-washed tomatoe from a s:
A 12 year old male was brought to us with history of fatiguability, vomiting and loose stools for 6 hours. There was no history of fever, convulsion, and altered sensorium. The vitals were stable except some dehydration. Investigations revealed hemoglobin 10.8g/dL, TLC 16.6×103/mL, platelet 360×103/mL, blood sugar 299g/dL, blood urea 28g/dL, S creatinine 0.9g/dL, Na 139 mEq/L,K 3.3mEq/L, pH 7.38, PaCO2 32 mmHg, PaO2 96 mmHg, and Bicarbonate 19 mEq/L. Urine showed sugar 4+ and moderate ketone bodies. In view of dehydration, hyperglycemia, glycosuria, ketonuria, low bicarbonate levels, DKA treatment protocol was started with IV fluids and insulin infusion. The level of consiousness deteriorated by 12 hours and Glasgow Coma Scale was 12. He developed fasiculations and jerky movement of limbs. His respiration was 28/min and shallow, heart rate 64/min, BP 110/70 mm of Hg, oxygen saturation 96%. His pupils were 2mm in size and were reactive. CT scan head was normal. Due to fasiculations and shallow respiration, organophosphorus intoxication was suspected and plasma cholinesterase was done; it was 550 U/L (Normal=2710-11510 U/L). The diagnosis was revised to organophosphorus intoxication and child was managed with atropine and pralidoxime. He responded well and was discharged after 6 days. Retrospectively, boy gave history of ingestion of 4 tomatoes in the field without washing 6 hours prior to admission.
The most common route of exposure to organophosphorus compounds is ingestion of agricultural products [1]. Probably our patient had poisoning from eating tomatoes contaminated with pesticide. Organophosphorus poisoning was not suspected at presentation, as the child presented to us with muscarinic symptoms like vomiting and diarrhea. Low levels of plasma choline-sterase support the diagnosis of OP poisoning [2]. Although plasma acetyl cholinesterase estimation was sufficient to support the diagnosis of organophosphorus poisoning in our case, we were unable to do estimation of RBCs ACE and urinary para-nitrophenol for technical reasons. Hyperglycemia is a known adverse effect of organophosphorus exposure and has been confirmed in animal studies [1,3-5]. The glucose metabolism is affected by several mechanisms, including oxidative stress, inhibition of paroxanase, stimulation of adrenal glands and release of catecholamines, and effect on metabolism of liver tryptophan [4]. In an earlier study glycosuria was observed in 69% of cases with OP poisoning. Organophasphorus intoxication can mimic DKA and its diagnosis may be delayed. Whenever there is discrepancy between clinical features and biochemical features in a suspected, DKA child, we should emphasize the need to look for an alternate diagnosis.
References
1. Levy-Khademi F, Tenenbaum AN, Wexler ID, Amitai Y. Unintentional organophosphate intoxication in children. Pediatr Emerg Care. 2007;23:716-8.
2. El-Naggar Ael-R, Abdalla MS, El-Sebaey AS, Badawy SM. Clinical findings and cholinesterase levels in children of organophosphates and carbamates poisoning.Eur J Pediatr. 2009;168:951-6.
3. Akyildiz BN, Kondolot M, Kurtoðlu S, Akin L. Organophosphate intoxication presenting as diabetic ketoacidosis. Annals Trop Pediatr. 2009;29:155-9.
4. Rahimi R, Abdollahi M. A review on the mechanisms involved in hyperglycemia induced by organophosphorus pesticides.Pesticide Biochemistry Physiology. 2007; 88:115-21.
5. Shobha TR, Prakash O. Glycosuria in organophosphate and carbamate poisoning. J Assoc Physicians India. 2000;48:1197-9.
JDepartment of Pediatrics
JSS Medical College, JSS University
Mysore, Karnataka, India
Comment from Stopspraying.org
Why it can take years to see health problems
from eating pesticides in food
 While pesticides are in nearly all non-organic foods you eat everyday, you may not personally notice the effects of the pesticides for decades. First, it's important to understand that some children have one-third lower levels of the liver enzyme known as cytochrome P-450. This enzyme works to detoxify pesticides and other chemicals in the body. People with lower levels of this enzyme would have chemicals remain in their blood for longer periods, thereby having more time to damage different organs and body systems.
While pesticides are in nearly all non-organic foods you eat everyday, you may not personally notice the effects of the pesticides for decades. First, it's important to understand that some children have one-third lower levels of the liver enzyme known as cytochrome P-450. This enzyme works to detoxify pesticides and other chemicals in the body. People with lower levels of this enzyme would have chemicals remain in their blood for longer periods, thereby having more time to damage different organs and body systems.
Also delaying the appearance of disease, many organs can sustain considerable damage before problems are noticed. For example, in type-1 diabetes, about 80% of the beta-cells in the pancreas must cease to function before diabetes symptoms appear. The human liver must sustain 70% damage before problems appear in routine blood tests. When this 70% threshold is reached, toxic chemicals stay in the body longer, thereby having more time to cause damage to other parts of the body - including the immune system.