BODY BROKEN
What malfunctions in the body that causes diabetes. Covers autoimmune - thymus damage - natural killer cells
INTRODUCTION
Why diabetes is more serious than other illnesses - discussion & summary of upcoming chapters.
THE NUMBERS
Compares diabetes rates today with rates years ago. Trends and disturbing predictions for tomorrow.
HEALTH PROBLEMS
Diabetes = 12 year loss of life - increased rates of blindness - heart disease - cancer - kidney loss.
CAUSES OF DIABETES
Study after study links diabetes to chemicals in home products - pesticides - cosmetics - food additives & more!
REMISSION
People experiencing true remission - defines honeymoon - suprising facts on beta-cell regeneration.
OBESITY LINK
Research finding same chemicals causing diabetes cause obesity. Discusses obesogens - how & why
REVERSING DIABETES
Time to take conclusions of scientists and put into real-time practice. Are doctors resisting?
CHAPTER REVIEW: While people with type-1 diabetes are well aware that their condtion is caused by 80-90% death of beta-cells in the pancreas, what isn't well known is what malfunctions inside the body that allows this to happen. This chapter focuses on just this topic and discusses the following three important areas:
1.
Malfunction of the thymus gland (which works vigorously to filter autoimmun cells)
2. Malfunction of natural killer cells
(which destroy autoimmune cells that attack the pancreas)
3. Malfunction of the ability to "scavenge" free-radicals (which leads to faster damage to the interior of cells - especially the mitochondria).
IF YOU ONLY KNEW:
A QUICK REVIEW OF WHAT GOES WRONG IN TYPE-1 DIABETES
Diabetes type-1 and type-2 don't just happen overnight, your body has been grooming you for the disease over the past 10-20 years, but unfortunately, you didn't know it. In this chapter you'll read how critical defense systems within the body slowly fail one after the other including the ability of the thymus to filter autoimmune cells - the ability of natural killer cells to remove autoimmune cells - and also the ability of your anti-oxidant systems (such as glutathione) to prevent damage to the interior of cells from free-radicals. When these three are too weak - autoimmune disesease such as diabetes come in like a lion.
Many scientists have openly stated, and logically so, that the first step in curing diabetes is to find out how to stop the malfunctioning immune system cells from attacking healthy body cells. No matter how many pancreas transplants are done in the operating room, if the autoimmune process isn't stopped, the transplanted pancreas will be destroyed as well. However, if we can find a way to restore quality function to the thymus and natural killer cells, the progression of diabetes would stop and possibly reverse (if beta-cells can regenerate in larger numbers than being destroyed). In summary, it is important to remember the one direct and two indirect causes of diabetes.
1. Autoimmunity (Immune System Attacks Pancreas)
2. Improperly Working Thymus (Inability to Filter Autoimmune Cells)
3. Malfunctioning Natural Killer Cells (Inability of the immune system to attack and "calm" autoimmune cells)
Understanding 1st Step in Autoimmunity - the hapten connection
It is now well documented that a weakened or defective thymus gland loses its ability to filter (remove) autoimmune cells from the blood, thereby resulting in more autoimmune cells remaining inside the body and increased damage to healthy tissue. All of this increases the likelihood of diabetes and other autoimmune diseases. Natural killer cells can take up a bit of the slack by removing autoimmune cells directly or by producing compounds such as interferon which can "calm" any other significant hyperactive autoimmune processes. However, natural killer cells themselves have been found to lose their ability to function properly after exposure to a number of petroleum chemicals, including pesticides. The question still remains, however - What happens first that causes immune system cells to become "ignorant" and begin attacking healthy tissue?
Haptens Form when Chemicals Attach to Proteins:
In this 2015 study, scientists at the Immunosciences Lab in Los Angeles have for the first time provided evidence on what appears to be happening within the body to start of the autoimmune process. This was all done by documenting immune system responses to 11 common chemicals and comparing this with immune responses to a mold called aflatoxin. Aflatoxin can produce toxic compounds and is found in small amounts in foods such as grains and peanuts. Once aflatoxin enters the body, it has been shown to bind onto proteins in the blood (such as albumin) which then attaches to healthy tissue. Immune system antibodies are then formed to attack this newly formed aflatoxin/protein combination, but unfortunately, also kills the healthy cell with it.
Which Chemicals Form Haptens?
A number of chemicals used in modern society are now being found to attach to proteins. When a chemical does connect to a protein, it forms a highly immune reactive compound called a "hapten." Since aflatoxin can form a hapten, scientists wondered if this could also occur with 11 other chemicals commonly used in consumer products. To explore this theory, scientists took blood samples from 400 healthy donors and exposed each sample to aflatoxin and then to 11 different chemicals. This included the chemical known as BPA (used in making plastic bottles and food can liners), the pesticide permethrin (used in indoor pest control - mosquito control and agriculture), a common flame retardant chemical used in computer circuit boards and also a benzene type chemical commonly found in car exhaust, gasoline and food coloring and many other consumer products.
Reduce Hapten Exposure Should Reduce Autoimmunity
Scientists then measured specific antibodies that were formed after exposure to these chemical/protein combinations and compared it to the level of antibodies formed after exposure to aflatoxin. The logic here being that if the chemicals caused the formation of similar levels of antibodies as did aflatoxin, then we could expect similar harmful autoimmune responses from the chemicals. After exposure to aflatoxin, blood samples showed an average 7% increase for both IgG and IgM antibodies. Interestingly, some of the 11 chemicals caused similar or greater immune responses. For example, the water bottle and canned food chemical BPA resulted in an average increase of 13% antibodies for IgG and IgM. The benzene ring chemical (as in gasoline and vehicle exhaust) resulted in an average 11% increase in antibodies. The flame retardant chemical used in computers resulted in an average increase of 15% for IgG and IgM antibodies. The pyrethroid pesticide permethrin had one of the largest increases averaging about 19% for both IgG and IgM antibodies. As can be seen here, the levels of antibodies against the chemicals increased which supports the idea that common chemicals may be a significant contribution to the increasing rates of autoimmunity (and potentially diabetes). In conlusion the researchers stated,
Vol. 35(4): 383-397,
April 2015
Immunosciences Lab, Inc.
Los Angeles, CA, USA
Dept. of Clinical Sciences
Bastyr University California
Dept. of Mathematics
Boise State University, USA
3 Autoantibodies as Primary Cause of Type-1 Diabetes
Autoantibodies are antibodies in the blood that have malfunctioned for some reason. Normally, antibodies attack foreign invaders such as bacteria or viruses. However, in type-1 diabetes, B lymphoctye white blood cells malfunction and produce antibodies against healthy insulin producting beta-cells of the pancreas. When autoantibodies attach to the beta cell, they act like magnets and attract other immune system white blood cells which then destroy the beta cell. This increased destruction of beta-cells continues for years until about 80% of beta-cells are destroyed, thereby resuting in diabetes (NOTE: New studies suggest that this is much less and closer to 50% at diagnosis.) The three primary autoantibodies identified that destroy beta-cells in the pancreas include:
| GADA Glutamic Acid Decarboxylase Autoantibody |
The GADA antibody attacks the GAD65 enzyme in beta-cells in the pancreas. GAD65 produces GABA which is involved in regulating insulin output. |
| IA-2 Islet Antigen-2 Autoantibody |
IA-2 is a major target for islet cell autoantibodies. The protein is found in up to 80% of children and adolescents with T1 diabetes. |
| IAA Insulin AutoAntibodies |
IAA's are autoantibodies that target insulin itself. They were present in 18% of 112 newly diagnosed type-1 diabetics prior to beginning insulin treatment. See 2nd journal listing in SCIENCE. |
Quote from researchers in the study: "... the current tests for autoantibodies to these three autoantigens are highly predictive of type-1 diabetes.
Vol. 54 (suppl 2.S52), Dec. 2005
Dr. Catherine Pihoker
Dept. of Pediatrics & Medicine
University of Washington
Seattle, Washington
1 of 5 Siblings of Diabetic Child
have Autoantibodies
Having 2 Antibodies = 90% Chance of
Future Diabetes
If your brother or sister has type-1 diabetes - you have about a 20% chance of having autoantibodies as well - that's one of the conclusions of this study conducted by the Diabetes Research Center in Finland. Since typically all children who develop type-1 have autoantibodies attacking their pancreas - having an accurate way to measure and predict future diabetes in siblings would be extremely helpful to doctors and families. Like a window to the future, this is now being accomplished by identification of different types of autoantibodies in childrens' blood. As discussed previously, type-1 diabetes occurs when the immune system malfunctions and mistakenly destroys beta-cells through different processes including making antibodies against the pancreas. In this study, researchers wanted to investigate if autoantibodies against the pancreas were higher in brothers and sisters of diabetic children, and therefore, help in predicting future diabetes. To answer this - 180 non-diabetic siblings of diabetic children were tested for four different autoantibodies. Children were all under age 6 at the time of testing. Antibodies tested included islet cell antibodies (ICA), glutamate decarboxylase antibodies (GADA), insulin autoantibodies (IAA), and antibodies called islet antigen-2 (IA-2A). After adding up the numbers, they found that nearly 20%of all siblings had one or more autoantibodies against their pancreas beta-cells. Breaking this down to individual antibodies, they found that 12% of the 180 children had islet cell antibodies - 7% had insulin antibodies - 8% had GADA antibodies, and about 8% were positive for the IA-2A antibodies. The next important thing to find out was how many different types of antibodies a child had, as having more than one antibody type greatly increases the risk of sooner appearance of diabetes. So, when looking further into the numbers - they found that 16 of the 180 children (about 9%) had one detectable antibody - 5 (about 3%) had 2 antibodies and another 12 children (7%) had 3 or more antibodies. These cooperative 180 children were then followed over the years until they reached age 10 to see how many developed diabetes. Results showed that 15 of the 180 children (18.3%) developed clinical type-1 diabetes sometime before age of 10. What's noteworthy about this, the ones who developed diabetes were the ones who typically had more than one of these renegade antibodies. For example, of the 15 children who developed diabetes, 13 were in the group that had 2 or more antibodies. Looking at this in another way - of the 17 children who tested positive for 2 or more autoantibodies - 15 of them (nearly 90%) developed diabetes before age 10. In other words, if your child had 2 or more pancreas autoantibodies, they had a 90% chance of developing diabetes within 5-7 years. Whether this percentage holds true for larger groups of children remains to be seen, but a number of studies are underway to find this out conclusively. One thing that can be taken from all of this is that autoantibodies play a significant part in taking the pancreas beta-cells out of action, but it also exposes a fascinating silver lining; If we can identify situations in our environment that cause autoantibodies to form, and we remove these "situations," we potentially set up the scenario where we can delay or prevent the onset of diabetes. For example, if we remove environmental situations known to increase autoantibodies, the patient's antibody count will decrease, thereby allowing for improved regeneration of beta- cells in the pancreas. In conclusion, the researchers stated,
Vol. 85(3): 1126-32
Department of Pediatrics
Diabetes Research Center
Medical School University of Tampere
Finland
Body's Autoimmune Filter Weakened by Pyrethroid Pesticide
You may not make the evening news, but your thymus gland is arguably the most important part of your body for preventing all autoimmune diseases - including diabetes. While originally thought to be important only in childhood and adolescence, the thymus has now been shown to play a crucial role in adults as well. Located in the central upper chest, your thymus functions as a "maturing and growth area" for many important immune system cells that attack viruses and cancer - but this is just the beginning, more recently, the thymus has been found to act as a "filter" - with the ability to remove millions of autoimmune cells from the body. Like a policeman giving a sobriety test to a drunk driver, your thymus literally tests immune system cells for their ability to identify self and non-self. If immune cells are smart and can recognize the difference between good cells (self) and bad (nonself such as viruses) - they are allowed back into the bloodstream highway. If the immune system cell fails the test, such as identifying healthy body cells as invaders, they are sent to the electric chair. This critical role clearly shows that any environmental circumstance that can damage or weaken the thymus police could potentially lead to out of control autoimmune cells running rampant in our bloodstream - resulting in severe negative health consequences (such as type-1 diabetes).
In this study, researchers at the Dept. of Environmental Toxicology at University of California wanted to find out if the common pyrethroid pesticide deltamethrin could damage the thymus in live animals. Deltamethrin is popular among pest control operators in the U.S. and is used in home pest control, agriculture and golf-courses. Animals were given a single injection of the pesticide at doses ranging from a low of 6 mg/kg to 50 mg/kg. The thymus was then removed from the animals after 24 hours and examined. Even at the lowest dose at 6 mg/kg - resulted in the thymus losing 22% of its weight after 24 hours with increased reductions in weight as dosages increased. The researchers then performed another test to see how time affected the thymus after pesticide exposure. After exposing animals to 25 mg/kg of deltamethrin for 24 hours, the thymus weight was reduced by about 41%. During the next two weeks, the thymus continued to shrink in size daily reaching a maximum 50% reduction in weight after 2 weeks. For a bit of good news - the thymus also demonstrated the ability to regenerate as it steadily regained about 1/3 of its weight after 35 days at which point the study was ended. In conclusion, the researchers said the reduction of weight to the thymus was due to the thymus cells being destroyed by the pesticide through a process known as apoptosis. While the thymus was in a steady pace of increasing weight when the study ended at 35 days, it is not known how much more the thymus would have regenerated after 2 months, 3 months, etc. This study further increases encouragement for potential reversal of diabetes as the organ that protects us from type-1 diabetes does show signficant potential to improve function, but only when circumstances shown to cause damage are removed.
Abstract - Full Text PDF
Vol 51: 447-454, 1996
Dept. of Environmental Toxicology
Intitute of Toxicology and Env Health
Center for Environmental Health Sciences
University of Califiornia
Davis, CA, USA
Autoimmunity Starts Here Damage to the Thymus Gland
Like deltamethrin, permethrin is also a pyrethroid pesticide commonly used in mosquito control - agriculture - and indoor and garden pest control. It is also used as a topical skin treatment for preventing insect and mosquito bites. In the second study listed at right, researchers applied a single topical dose of the pesticide permethrin to the shaved skins of 5 week old mice in gradually increasing doses. As found with deltamethrin in the study above, permethrin also showed the ability to decrease the number of thymus cells - with 52% destruction of the thymus from 15 microl of the permethrin and 80% thymic destruction from 25 microl of permethrin. This major destruction to the thymus occurred after just a single permethrin skin application. In a real life situation - children often receive permethrin applications many times a week and in some cases daily.
Vol. 19(6), 383-389, Nov 2000 Food Chemical Toxicology
Vol. 40(12): 1863-73, Dec 2002
This Part of Beta Cell Involved in Insulin Release - GAD65 & GABA
As mentioned above, GAD65 is an enzyme in beta-cells that produces the compound known as GABA. Increased levels of GABA then result in increased insulin secretion by beta-cells.
QUOTE FROM STUDY AUTHORS: ... autocrine GABA, via activation of GABAARs, depolarizes the pancreatic β-cells and enhances insulin secretion. On the other hand, insulin down-regulates GABA-GABAAR signaling presenting a feedback mechanism for fine-tuning β-cell secretion.
October 21, 2011
Dr. Paul Bansal, et al.
Departments of Physiology & Medicine
University of Toronto, Canada
Vol. 36(11):847, November, 2011
Acceleration of Type-1 Diabetes if IA-2 Autoantibodies Present
IA-2 is a beta-cell damaging antibody known as the insulinoma-associated protein-2. The function of the protein remains unclear but appears to be involved in enhancing insulin secretion. The frequency of IA-2 is similar in the USA and Europe and ranges between 60-80% in newly diagnosed type-1 diabetic patients. Children positive for IA-2 autoantibodies have accelerated progression of type-1 Diabetes.
Autoantibody Levels Lower After 12 Years
Scientists at Lund University in Sweden wanted to determine if there was a relationship between beta cell function and levels of autoantibodies in diabetic patients at diagnosis and then 12 years after diagnosis. The study was conducted with 107 adult diabeteic patients between the ages of 21 and 73. Results showed complete beta-cell failure (as measured by C-peptide testing) occurred only in patients who had islet antibodies at diagnosis. This included 77% of patients with multiple antibodies (16 of 21) and 80% of those with GADA antibodies (4 of 5). Interestingly, while most GADA positive patients still remained GADA positive after 12 years, patients with two or three antibodies at diagnosis had significantly lower levels of antibodies after 12 years. In keeping with this, the percentage of patients positive for all 3 islet autoantibodies decreased from 37% of patients at diagnosis to only 15% after 12 years. Among patients with two or three islet antibodies at diagnosis, complete beta-cell failure (undetectable fasting P-C-peptide) was present in 74% of patients (20 of 27) after 5 years
Vol. 51(6): 1754-62, June 2002
Department of Endocrinology
Lund University
Malmo University Hospital
Malmo, Sweden
Test Determines Insulin in Blood -
Identifies Type-1 or 2 Diabetes
Also Measures if Diabetes
is Worsening or Improving
It has typically been reported that 80-90% of all beta-cells in the pancreas are damaged at the time of type-1 diabetes diagnosis. However, this number has been challenged with new autopsy studies published in 2017 found this number is actually closer to 50-60% in type 1 diabetes for adults but . Whether it is 90% or 50%, the remaining beta-cells still have the ability to produce some insulin. Insulin output can be measured in patients through a blood test known as C-peptide. When beta-cels are in the process of making insulin, C-peptide is produced as a by-product. Therefore, the amount of C-peptide in the blood can be used to accurately determine the amount of insulin being made by beta-cells. The C-peptide test can also be used to help determine if the patient has type-1 or type-2 diabetes as patients with higher C-peptide would be more likely to have type-2 diabetes. Patients with type-1 diabetes can also be given the C-peptide test yearly to determine if their beta-cells have stopped producing insulin or have improved insulin production (via regeneration of pancreas or reduction of autoantibodies). Rather than measure direct insulin in the blood, it is preferable to measure C-peptide as it does not get metabolized by the liver (which does occur with insulin) Depending on the measurement criteria, normal reference ranges for C-peptide are 0.8 - 3.1 ng/ml or 0.26-1.03 nmol/L.
C-Peptide Blood Test
Type 2 Diabetes Being Redefined as Autoimmune Disease
While type-1 diabetes is an autoimmune disease in which the immune system mistakenly destroys the pancreas, type-2 diabetes has long been considered only a metabolic disorder - having nothing to do with autoimmunity. However, evidence now shows this is no longer the case. In new research from Stanford University School of Medicine, type-2 diabetes is also being shown to be an autoimmune disorder. In one part of the study, lead author Dr. Shawn Winer, found that immune system T-cells and B-cells begin attacking healthy tissue in mice when their fat cells grow too quickly. When the scientists used mice that lacked these B-cells, the obese mice did not develop insulin resistance. The scientists then carried this research to humans. Here they studied 32 age and weight matched overweight people who differed only in their sensitivity to insulin. When comparing the two people in each group of same weight (one with insulin resistance and the other without) the researchers stated, "We were able to show that people with insulin resistance make antibodies to a select group of their own proteins. In contrast, equally overweight people who are not insulin-resistant do not express these antibodies. Dr. Winer, then went on to state,
Defective Natural Killer Cells in Children with Type 1 Diabetes
Since children with higher levels autoimmune antibodies are the ones who get diabetes, the next question is - why do only some children have this problem and not others? To answer this question, scientists at Jilin University in China investigated the quality and numbers of natural killer cells in children with diabetes. For a quick review - natural killer cells are your body's first line of defense against viruses and cancer cells, which is why it makes sense that people with lower numbers of natural killer cells have higher rates of cancer and virus infections. These powerful microscopic cells make up only a small percentage of your immune system's total white blood cells. What is interesting in relation to diabetes, these powerful little inventions have also been found to have a superb talent for fiding and destroying autoimmune cells. This means that someone with properly working natural killer cells is able to have a lower amount of auto-antibodies since the natural killer cells are working for the team. This certainly brings up the theory that children who get diabetes may have a problem with their natural killer cells.
To see if this in fact was a problem, doctors at the Department of Endocrinology at Weihai Municipal Hospital in China tested 30 children and adolescents with type-1 diabetes and compared their natural killer cell numbers to 27 healthy children without diabetes. Results showed that newly diagnosed diabetic children had a significantly lower percentage of natural killer cells. Along with this, the natural killer cells the children did have were secreting less of an important compound known as interferon. In conclusion, the scientists stated,
Vol. 44(2), 180-190, Feb 2017
Dept of Central Laboratory
Jilin University, Changchun, China
Immune System's Natural Killer Cells Critical for Protecting You from Diabetes
Mice were were exposed to the chemotherapy drug cyclophosimide which is known to cause diabetes in test animals. It was found that some mice quickly developed diabetes and others showed no signs of diabetes. When looking at specifics in their immune systems, it was found that mice that stayed healthy (and did not develop diabetes) had higher numbers of natural killer cells and their natural killer cells also produced higher levels of interleukin-4 (IL-4). Interleukin-4 is one of the ways in which white blood cells communicate to other white blood cells. As lower numbers of natural killer cells are suspected of increasing diabetes, this raises the question as to whether any environmental factors appeared which could potentially lower the number and/or quality of natural killer cells.
Vol. 188(10), 1831-1839, Nov 1998
Department of Molecular Biology
Princeton University, New Jersey
Autoimmunity Improves via Natural Killer T Cells
Natural killer T cells are slightly different than the more common natural killer cells. Natural killer T cells are less common than natural killer cells and comprise only about 0.1% of all blood T cells. They have the unique ability to produce large amounts of cytokines which has the ability to communicate with other immune cells and also suppress immune system response. Think about the importance of this. These unique natural killer T cells have the able to suppress (or lower) immune system response. So, if someone has an overactive immune system resulting in autoimmunity against beta-cells (or any organ in the body), it is certainly nice to have natural killer T cells around to quiet the masses.
In studies of patients and mice with a variety of autoimmune diseseases, the number and functions of natural killer T cells is reduced. In experiments with mice, it was found that a deficiency of natural killer T cells worsens autoimmune conditions (such as diabetes). Therefore, one would expect that someone who has a lower number of natural killer T cells would have less ability to "calm down" autoimmune reactions within the body, and consequently, receive a higher rate of tissue damage from autoimmune reactions within the body.
Vol. 9(1): 4-14
Dept. of Microbiology & Immunology
Vanderbilt Univ. School of Medicine
Nashville, TN USA
Rapid Progression of Type-1 Diabetes
Occurs
if patients have low numbers of some types of natural killer cells
Although the immune system's lymphocyte T cells play a key role in beta-cell destruction in the pancreas, researchers were finding other immune system cells were malfunctioning and contributing in the all out assault on the pancreas. Normally, cells called regulatory T cells (Tregs) and invariant natural killer T cells (iNKT for short) have the job of maintaining what is called "periperhal tolerance." This simply means their job is to insure everyone on the immune system team plays by the rules and and tolerates normal body cells. So, basically, the Tregs and iNKTs make sure everyone is friendly. However, in patients with type-1 diabetes, it was found their Tregs and iNKT's were lower in number and performing abnormally. In fact, when researchers artificially increased the number of iNKT cells in animal studies, the animals showed a decrease in type-1 diabetes. When mice had high levels of iNKT cells, diabetes wasn't a problem. In fact, researchers were able to pinpoint what was wrong with these previously normal functioning cells. Apparently, crowd control goes south with the cells no longer can produce enough of two compounds known as interleukin-13 and interleukin-14 - We'll call them IL-13 and IL-14 for short. Excuse this next analogy, but IL-13 is like mace that allows iNKT cells to calm down any other cells in the area that are thinking about attacking teh beta-cells in the pancreas. Although the authors in this study state there is no therapy to revent type-1 diabetes, they do state that if we can determine the origin (cause) of iNKT cell alteration, it would represent a new path to intervene before type-1 diabetes and the information provided in this book is attempting to do just that.
Vol. 65(8): 2121-2123, August 2016
These Immune Cells Both Destroy and Protect the Pancreas
This study reviewed the research on how the immune system damages the pancreas.
While we hear much about autoantibodies, here are two key points from this article.
1. T Regulatory Cells (called Tregs) prevent diabetes
(animals deficient have accelerated diabetes onset).
2. Patients with diabetes have impaired function of natural killer cells.
Vol. 10: 501, July 20, 2010
Immune cell crosstalk in T1D
Macrophage Malfunction:
Another Autoimmune Step to Diabetes Type-1
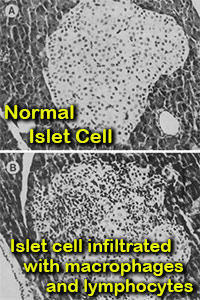 Macrophages are a type of white blood cell in the immune system.
In conclusion, the scientists stated, Along with cells called dendritic cells, macrophages are number 1 among cells that present signals (antigens) to other cells to mount an attack. Researchers in this study found an interesting observation among mice genetically prone toward diabetes type-1. When mice were exposed to a compound known to cause diabetes, the islets in their pancreas (islets hold insulin producing beta-cells) became flooded with macrophages and other immune system cells in a process known as insuliltis (see picture). They also found that by reducing macrophages (through exposure to silica), there was a dramatic decrease in function and numbers of T lymphocytes and natural killer cells - resulting in prevention of the pancreas beta-cell destruction. The authors quoted other studies showing that natural killer cells and helper and cytotoxic T lymphocytes are actively involved in the destruction of islet cells (paragraph 3, Pg.585).
Macrophages are a type of white blood cell in the immune system.
In conclusion, the scientists stated, Along with cells called dendritic cells, macrophages are number 1 among cells that present signals (antigens) to other cells to mount an attack. Researchers in this study found an interesting observation among mice genetically prone toward diabetes type-1. When mice were exposed to a compound known to cause diabetes, the islets in their pancreas (islets hold insulin producing beta-cells) became flooded with macrophages and other immune system cells in a process known as insuliltis (see picture). They also found that by reducing macrophages (through exposure to silica), there was a dramatic decrease in function and numbers of T lymphocytes and natural killer cells - resulting in prevention of the pancreas beta-cell destruction. The authors quoted other studies showing that natural killer cells and helper and cytotoxic T lymphocytes are actively involved in the destruction of islet cells (paragraph 3, Pg.585).
Vol. 39(5): 590-596, May 1990
Julian McFarlane Diabetes Research Ctr
University of Calgary
Alberta, Canada
Vol. 189(2): 347, January 1999
Julian McFarlane Diabetes Research Ctr
University of Calgary
Alberta, Canada
How Natural Killer Cells & Thymus Gland Prevent Diabetes & other AutoImmune Disorders
As described in the research above, islet cells in the pancreas are flooded with macrophages prior to development of diabetes and subsequent destruction of beta-cells. It has also been found that patients with diabetes and those with other autoimmune disorders are highly predisposed to the development of macrophage activation syndrome (MAS).
Below are the main points about this syndrome:
1. Macrophage activation syndrome is caused by hyperactivation of the macrophage immune response as a consequence of impaired natural killer cell function. In a population of patients with autoimmune disorders, type-1 diabetic patients are extremely predisposed to this syndrome. Pg. 472, par1)
2. Environmental factors are necessary to trigger the development of autoimmune disorders. Under normal conditions, the thymus prevents the complete development of autoimmune lymphocytes due to the mechanism of central tolerance. Nonetheless, small pools of autoreactive cells escape from the selection to peripheral circulation. As a back-up, there are also peripheral mechanisms (peripheral self-tolerance) aimed at destroying autoreactive lymphocytes. If central or peripheral tolerance mechanisms fail, immune reaction to self antigens can initiate autoimmunity [see study].
3. Natural killer cells have the ability to destroy lymphocyte cells attacking the pancreas. They do this by attaching onto the autoimmune T cell - and then releasing granules containing perforin and granzymes B into the T cell. This results in very fast destruction of the autoimmune T cell.
4. To quote the authors directly (pg471, par1), "Impaired action of perforin, disturbed degranulation process or defects in Fas/FasL-dependent apoptosis pathway may lead to the loss of natural killer cells function and to development of autoimmune disease.
View Online - Download PDF
Vol. 40(4): 470-476, Jan 2015
Medical University of Warsaw
Poland
Excellent Review of Natural Killer Cells in AutoImmune Disorders
In another report, scientists conducted an extensive review of research investigating the role played by natural killer cells in protecting us from diabetes and other autoimmune disorders. Below are direct quotes from their report:
1. Cytokine activated human NK (natural killer) cells can directly kill both activated macrophages and T Cells.
2. Impaired NK cell function is frequently seen in patients with autoimmune disorders.
3. Over the last 30 years, many studies have reported decreased NK cell numbers or impairment of NK cell cytotoxicity in the peripheral blood of patients with autoimmune diseases such as multiple sclerosis (MS), rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), Sjögren's syndrome, and type I diabetes mellitus (T1DM)
4. ...more recent studies have also clearly identified an association between bona fide NK cell deficits in the peripheral blood with many autoimmune disorders [55] including autoimmune thyroid disease [56, 57] and psoriasis [58] as well as a number of pediatric rheumatologic diseases including juvenile dermatomyositis [59] and systemic-onset juvenile idiopathic arthritis (JIA) [60].
5. ...these reports raise the possibility that autoimmunity may be associated with NK cell numeric or functional deficiencies.
6. ...several studies have demonstrated accumulation of NK cells in affected tissues of autoimmune patients. For example, infiltrating NK cells have been found to accrue in the pancreatic islet of T1DM patients [64], the hair follicle of patients with alopecia areata [65], and the muscle of children with juvenile dermatomyositis [66, 67]
7. Interestingly, CD56 bright NK cells, in particular, accumulate in the skin lesions of psoriatic patients [68] and the synovium of RA patients [69, 70]. These observations support the hypothesis that decreased NK cells in the peripheral blood of patients with autoimmune disorders may reflect the trafficking of NK cells to affected tissues.
8. Furthermore, studies in T1DM have demonstrated modestly decreased NK cell numbers in the peripheral blood of patients with recent-onset T1DM but not in patients with long-standing T1DM [72]. Interestingly, NK cells were identified around the islet cells of a subset of patients with recent-onset T1DM [64] but not in postmortem pancreatic samples from T1DM patients with long-standing disease [73]. Murine models of T1DM have also demonstrated localization of NK cells near islets as well as a temporal correlation in NK cell infiltrates during the development of diabetes, with a greater influx of NK cells during the prediabetic stage compared with late diabetes [74, 75, 76].
9. ...chronic NK cell lymphocytosis (increased numbers of immature NK cells) is associated with autoimmune syndromes, including vasculitis, arthritis, and peripheral neuropathy [82, 83, 84]. This disorder provides evidence that the dysregulation of NK cell homeostasis in the context of decreased NK cell cytotoxicity may contribute to the onset of autoimmunity.
10. Natural Killer (NK) cell activation is regulated through several disinct mechanisms to prevent inappropriate responses. First, they express inhibitory recptors that recognize widely expressed ligands. Second, the up-regulaton of host ligands for activating receptors is regulated to prevent inadvertent damage to normal health tissue. Finally, full NK cell responsiveness requires "licensing" through inhibitory receptors, which prevents the unrestrained activation of NK cells that do not express appropriate self-MHC class I-reactive inhibitory receptors. For people without a degree in immunology, this simply means that natural killer cells possess several ways to prevent them from attacking healthy tissue.
Vol. 15: 216, July 2013
Drs. L Fogel, W Yokoyoma, A French
Division of Pediatric Rheumatology
Washington University
Natural Killer Cells Destroy Macrophages Linked to Starting Type-1 Diabetes
While the thymus gland works as the body's initial filter for removing autoimmune cells, there appears to be a "back-up" system ready to go in case the first defense goes on the blilnk. In this study, researchers demonstrated that human macrophages have the ability to activate natural killer cell proliferation and "prime" natural killer cells to kill target cells. On the flip side, they also found that natural killer cells also have the ability to directly kill autoimmune related macrophages. In conclusion the researchers stated,
Vol. 109(9): 3776-85, May 2007
Division of Cell & Molecular Biology
Imperial College London, UK
While the section above described how defects in natural killer cell function can cause autoimmune disorders such as diabetes, this next section will investigate studies showing damage to natural killer cells from chemicals in the environment.
Natural Killer Cells Damaged by Mosquito Control Pesticide Naled Links to Diabetes and Autoimmune Disorders
Natural killer (NK) cells are critical for preventing viruses from host infection as well as preventing cancer. Loss of function or numbers of these cells increases rates of high viral prevalence and more aggressive cancers. NK cells have also been found to play a large role in preventing autoimmune disorders by attacking T cells showing autoimmunity toward the pancreas. Therefore, any situation that damages natural killer cell number or function has the potential for accelerating the onset of autoimmune disorders such as diabetes. In this study, scientists investigated if the pesticide dichlorvos (a breakdown product of Naled/Dibrom) and the common agricultural pesticide lorsban (chlorpyrifos) were able to damage natural killer cells. Natural killer cells were treated with both dichlorvos and chlorpyrifos at levels from 0 to 100 parts per million for 1 to 72 hours. Results showed that both pesticides caused destruction of natural killer cells through a process known as apoptosis in a time and dose-dependent manner. Chlorpyrifos showed a faster response than dichlorvos at higher doses; whereas, dichlorvos showed a slower, but stronger apoptosis-inducing ability at lower doses.
Vol. 239(1-2):) 89-95, July 2007
Dept. of Hygiene & Public Health
Nippon Medical School,
1-1-5 Sendagi, Tokyo, Japan
Pesticides Weaken Ability of Natural Killer Cells
to Destroy Cancer
Same Pesticides found in Indoor Air of Homes
built before 1989
Alhtough this study is done with cancer and not diabetes, it is important to include here because it shows how natural killer (NK) cells can be damaged by pesticides and NK cells also play a critical role in protecting us from autoimmune diseases including diabetes.
NK cells play a central role in your immune defense against tumor development and viral infections. Thus, any agent that interferes with the ability of NK cells to lyse (kill) their targets could increase the risk of tumor incidence and/or viral infections [author quote from Abstract]
In this study, scientists tested 11 different pesticides to see if they were able to weaken the ability of natural killer cells to destroy cancer cells in a laboratory setting. The compounds were tested in both purified NK cells as well as a cell preparation that contained lymphoctye T cells) and NK lymphocytes (referred to as T/NK cells). Lymphocytes were exposed to the compounds for periods of time ranging from 1 hour to 6 days.
Results showed that exposure of highly purified NK cells to 5 micrograms per cubic meter of different pesticides for 24 hours greatly weakened their ability to remove and destroy cancer cells. Below is a breakdown of specific pesticides and their reduction in cancer killing capacity of the NK cells.
| alpha-chlordane | 88% reduction in NK killing ability |
| gamma-chlordane | 92% reduction in NK killing ability, |
| DDT | 61% reduction in NK killing ability |
| Heptachlor | 64% reduction in NK killing ability |
| Oxychlordane | 69% reduction in NK killing ability |
| Pentachlorophenol (PCP) | 76% reduction in NK killing ability |
The loss of cancer killing ability with alpha-and gamma-chlordane remained essentially constant for 6 days, while that seen with DDT, oxychordane and PCP increased with longer exposures. PCP was the most effective of the compounds tested at decreasing NK function. Of the compounds that caused decreased cancer killing when tested in purified NK cells, PCP and oxychordane also decreased the cancer killing ability of T/NK cell preparation. In conclusion, the researachers stated,
Tennessee State University
Nashville 37209, USA.
CHEM-TOX NOTE: Of signficant concern, the pesticides chlordane and heptachlor are still routinely found in indoor air of homes built before the compound was banned in 1989. Also, homes built before 1980 have been found to have significantly high levels of chlordane and heptachlor as the pesticide was frequently used inside homes in monthly pest control operations.
Vol 23(10): 463-471, October 2004
Dept. of Chemistry
Tennessee State University
Nashville, TN, USA
Flame Retardant Severely Weakens Immune Natural Killer Cells
Vol. 6(4), Oct 5, 2009
Triphenyltin Pesticide Causes Severe Damage to Natural Killer Cells
Triphenyltin is a fungicide used in paints on the bottom of boats and as a pesticide in agriculture. In this study, scientists exposed freshly isolated white blood cell lymphocytes to triphynyltin compounds at levels of 750nM for 1 hour in a test tube. This resulted in a 63% decrease in natural killer cell cytoxic function. This means natural killer cells destroyed 63% less cancer or virus infected cells. Scientists then wanted to see if time would restore their ability. To test this, after exposure to the 750nM triphenyltin, they put the natural killer cells into a clean environment free of triphenyltin. After 6 days - results showed they had weakened even further and had a 91% reduction in cytotoxic ability.
CHEM-TOX COMMENT: Although not related specifically to diabetes, this study is included because of the critical importance being found of natural killer cells and their ability to eliminate autoimmune cells. Also, this study shows that while an initial test may not show immune system effects from a chemical, it is important to continue testing through a significant time period as effects can show up days following exposure.
Vol. 92(3): 213-2120, August 2003
Dept. of Chemistry
Tennessee State University, USA