REMISSION
People experiencing true remission - defines honeymoon - suprising facts on beta-cell regeneration.
INTRODUCTION
Why diabetes is more serious than other illnesses - discussion & summary of upcoming chapters.
THE NUMBERS
Compares diabetes rates today with rates years ago. Trends and disturbing predictions for tomorrow.
BODY BROKEN
What malfunctions in the body that causes diabetes. Covers autoimmune - thymus damage - natural killer cells.
HEALTH PROBLEMS
Diabetes = 12 year loss of life - increased rates of blindness - heart disease - cancer - kidney damage
CAUSES OF DIABETES
Study after study links diabetes to chemicals in home products - pesticides - cosmetics - food additives & more!
OBESITY LINK
Research finding same chemicals causing diabetes cause obesity. Discusses obesogens - how & why.
REVERSING DIABETES
Time to take conclusions of scientists and put into real-time practice. Evidence for rapid improvement.
Evidence that Beta-Cells Regenerate - Curing Diabetes?
In a moment, you'll read a case-report of a 35 year old woman who was completely cured of type-1 diabetes. While her situation is unusual, it needs to be studied to see if anything can be learned that might give insight for being duplicated again. If nothing else, this woman demonstrated that insulin production in humans has the ability to increase dramatically, and her improvement most likely occurred because of significant new growth of beta-cells in her pancreas.
Before explaining this woman's circumstance, it is important you first understand the following research conducted at the Islet Research Center at the University of California in Los Angeles. In this 2005 study, Dr. J Meir and colleagues wanted to find out if there was evidence of new beta-cell growth in people who had type-1 diabetes for years and even decades. The premise being that if someone was able to grow new beta-cells after diabetes diagnosis, it lays out the possibility that type-1 diabetes can be cured, if there was some way to also reduce the immune system's attack on these newly formed beta-cells. Unfortunately, the answer to this question cannot be found from testing living humans since it requires detailed microscopic examination of the pancreas. Therefore, to conduct a study to answer this question, scientists inspected the pancreas' from 56 people (ages 4 to 67) who died an accidental death. Forty-two of these individuals had type-1 diabetes and fourteen did not have diabetes. After completing their inspection, they found 88% of those with type-1 diabetes had evidence of beta-cells. Researchers also wanted to look for evidence of recently destroyed beta-cells, as this would provide evidence that new beta-cells must growing from somewhere - otherwise the ongoing destruction would quickly eliminate all beta-cells.
To estimate the number of destroyed beta-cells, they used a special stain that 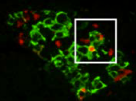 makes broken DNA fragments from the destroyed beta-cells appear bright red under a microscope. What they found was that all people with type-1 diabetes who had live beta-cells had evidence of ongoing beta-cell destruction as shown by the red dye (see picture showing both green beta-cells and red destroyed beta-cells). Truly remarkable was that beta-cell destruction was evident even in those with diabetes for 60 years (thereby implying they had also been experiencing beta-cell regeneration for 60 years). Also in proximity to the destroyed beta-cells were increased numbers of immune system cells called macrophages and T-Cells (thereby, suggesting they may have been involved in the beta-cell destruction). In conclusion the researchers stated,
makes broken DNA fragments from the destroyed beta-cells appear bright red under a microscope. What they found was that all people with type-1 diabetes who had live beta-cells had evidence of ongoing beta-cell destruction as shown by the red dye (see picture showing both green beta-cells and red destroyed beta-cells). Truly remarkable was that beta-cell destruction was evident even in those with diabetes for 60 years (thereby implying they had also been experiencing beta-cell regeneration for 60 years). Also in proximity to the destroyed beta-cells were increased numbers of immune system cells called macrophages and T-Cells (thereby, suggesting they may have been involved in the beta-cell destruction). In conclusion the researchers stated,
Astounding Remission of Type-1 Diabetes in Prison Inmate
How often does remission occur for someone with type-1 diabetes? Is it 10% - 50% - 1% or not at all. Although the percent experiencing remission is practically zero, if one person can do it, it implies others can achieve it as well - we just need to be a little smarter. In fact, new research is suggesting that there appears to be more things than we realized that can be done to decrease autoimmunity - improve beta-cell regeneration and achieve remission.
After an in-depth search through the literature for documentation and examples of remission cases for type-1 diabetes, there were reports of only two that I was able to find over several decades. For example, doctors here report a very interesting case in which a 32 year old woman experienced complete remission of type-1 diabetes. She was originally diagnosed with diabetes after being admitted to the hospital with symptoms of blurred vision and general stomach and chest pain. Her test results showed a random blood glucose of 938 mg/dl, an A1C of 12.7% and a +2 on the urine ketones dipstick test. Her GAD antibody assay was more than 4 times above normal at 0.09 (normal is ›= 0.02 nmol/L). Her C-peptide level (c-peptide is used to determine insulin production) was a little below normal at 0.70 ng/ml (normal is 0.78 to 5.19 ng/mL). After release from the hospital she was on basal bolus insulin and was taking her insulin as prescribed. After 4 months, an incident occurred in which the woman was then sent to prison and was for whatever reason, was not given any insulin while in prison. In a situation such as this we would expect the person to undergo rapid increases in blood glucose and a return of ketoacidosis. Interestingly, this didn't happen. She had no symptoms of hyperglycemia or ketoacidosis while in prison. After 7 months she was released at which point she contacted her doctors. At her medical follow-up immediately after being released (and not taking any insulin for 7 months), her A1C was 5.6% and fasting blood glucose was 98 mg/dl. She did have an unintentional weight gain of 14 pounds since the orignal diagnosis. In subsequent checkups, a little more than a year after her diagnosis, she was still in complete remission and not requiring any insulin therapy. This demonstrates another case in which someone with severe type-1 diabetes (A1C of 12.7%) was basically "cured" of their condition. It is interesting to note that the remission occurred only after being removed from her normal surroundings and being placed into a new environment and after not receiving insulin. As the research has now clearly demonstrated that diabetes can be caused by environmental sources that weaken or damage the body's defenses, it would have been enlightening to determine if something occurred at this woman's home that preceded her diabetes - such as the use of pesticides, etc.
FULL TEXT
Vol. 5(5): 28709, Oct 2015
College of Medicine
University of Illinois, USA
Mamatha Medical College, India
19 Year Old Young Man Experiences Remission of Type-1 Diabetes
Another case of diabetes remission occurred in this 19 year old patient who entered the hospital with ketoacidosis, a fasting blood sugar of 432 mg/dl and an A1C of 12.3%. He was also positive for the beta-cell autoantibodies called GAD (glutamic acid decarboxylase) which were measured at 46 units/ml. He began an intensive program of both insulin glargine and insulin glulisine at the prescribed dose of 0.5 units per kg body weight. After one month, the young man began to show lower glucose levels so doctors began reducing his daily insulin injections. This pattern continued and by 8 weeks he no longer needed insulin and entered complete remission with fasting glucose of between 70 and 130 and an A1C of 7.8%. At a one year follow-up, he was still in complete remission with an A1C of 5.8% and fasting glucose of 108 mg/dl. His fasting C-peptide was 1.0 ng/ml and a 75 gram glucose test was 152 mg/dl after 2 hours with a C-peptide of 4.3 ng/ml. After 15 months taking the drug sitagliptin only, he had an A1C of 6.3% and fasitng glucose of 122 mg/dl. GAD antibodies were still positive at 6 units/ml.
FULL TEXT
Vol. 2014(2014):140072, Sep 1, 2014
Universidad de Orient
Venezuela
Children's Hospital Oakland Res. Inst
Oakland, CA, USA
9 Year Old Boy Off Insulin after Beginning Paleolithic Ketogenic Diet
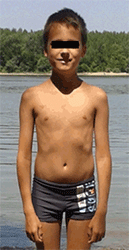 In December, 2013, this child was diagnosed with type-1 diabetes with a glucose level of 692 mg/dl and glucose in urine. He also tested positive for GAD autoantibodies (1280 IU/ml). He was placed on an insulin therapy of 21 units for six meals containing 210 grams of carbohydrates. He was on conventional insulin therapy for six weeks. Although he followed the prescribed diabetes diet and insulin treatment, his glucose levels fluctuated considerably. This resulted in his parents looking for alternative treatments.
In December, 2013, this child was diagnosed with type-1 diabetes with a glucose level of 692 mg/dl and glucose in urine. He also tested positive for GAD autoantibodies (1280 IU/ml). He was placed on an insulin therapy of 21 units for six meals containing 210 grams of carbohydrates. He was on conventional insulin therapy for six weeks. Although he followed the prescribed diabetes diet and insulin treatment, his glucose levels fluctuated considerably. This resulted in his parents looking for alternative treatments.
The diet was introduced gradually over a 5 day period. During this time insulin was adjusted according to fingerstick glucose measurements and beginning on the 6th day (February 18, 2014) the child was on the full Paleolithic ketogenic diet. To measure insulin output, doctors performed the C-peptide test again with results of 1.1 ng/ml. This is within the normal range of 0.9 - 7.1 ng/ml. Since glucose was normal before and after meals, the doctors stopped his daily insulin injections. Not only did this child have much more stabilized blood sugar levels but also experienced complete elimination of low blood sugar which was frequent while on insulin. After being on his new diet for 19 months his A1C levels were between 5.2 and 5.6%.
Vol. 6(12): 752-757, 2015
Evolutionary Medicine Working Group
Budapest, Hungary
Dept. of Neurology
University of Pecs, Hungary
Honeymoon - Partial Remission: What is this Exactly?
Parents often hear doctors refer to something called the "honeymoon period" after a child has been diagnosed with type-1 diabetes. This is a patient-friendly term that means the person is showing signs of improved pancreas insulin output and therefore requires less insulin. Not all children are lucky enough to achieve a "honeymoon." Numbers from different studies show only about 50-70% of children diagnosed with type-1 diabetes bounce into the honeymoon, with the lower percentage going with children under age 5 and the higher percentage going with older children. The honeymoon period usually begins one month after diagnosis and peaks at 3 months. It is believed to occur because of improved new beta-cell growth within the child's pancreas. It then begins a gradual decline month after month with most children ending the honeymoon after 9 months. Apparently, different doctors use different criteria to define the honeymoon period. Using the latest definition (called insulin dose-adjusted A1C), about 60% of children are in the honeymoon 3 months after diagnosis - 50% at 6 months - and only about 25% are honeymooning at 12 months. The term partial-remission is also used to describe the honeymoon period, therefore, both terms refer to the same observation. Some facilities describe the honeymoon (partial remission) as having an A1C of 7.5% or less while others define it as an A1C of 6% or lower. For those not familiar with diabetes, the A1C (same as HbA1C) is considered a more accurate way to measure blood glucose since it basically measures the amount of glucose that has been stored by our red blood cells. This number is used to give us more of an average blood glucose level over the past 6-8 weeks, rather than just one day. Six to eight weeks is the lifespan of a red blood cell and red blood cells act like a sponge to gradually soak up glucose during their short life span.
Another definition used to describe the honeymoon period is when the child has a daily insulin dose in units that is less than half their weight in kilograms. For us Americans, that means hitting the internet to first convert pounds into kilograms. For example, a 120 lb child has a weight of about 54 kilograms. If the child is taking less than 27 units of insulin daily (27 is half of 54), then he/she would be considered in partial remission (or experiencing a honeymoon).
One of the newest definitions of partial remission (and takes a little more time to calculate) was proposed by Dr. Henrik B. Mortensen at the Glostrup University Hospital in Denmark. Their method is called IDAA1C which stands for insulin dose-adjusted A1C. This is a mathematical formula that first calculates the daily dose of insulin in units per kilogram for the child and multiplies this by 4, and then adding this to the child's A1C%. Yes, I know I lost you on that, but here's an example to make it easier to undersand. My son has a weight of 124 lbs which is about 56 kilograms. He takes about 12 units of insulin daily including his nightime Lantis. Bringing out the calculator, we are going to divide the 12 units by 56 kilograms. So, we type in 12, press the divide symbol and then hit 56. This gives us the decimal 0.47. Next, we multipy .47 x 4 and get 1.8. The final step is to add this 1.8 to his last A1C of 5.5 which gives us a score of 7.3. Since anything less than 9 is considered partial remission, we can say that my son Alan is still in his honeymoon (or partial remission) after having diabetes for 10 months. This latest definition for partial remission is a little more difficult to calculate but is said to be more accurate at predicting actual insulin production. How long does the honeymoon last? Only 25% of those who reached the honeymoon at all are still there after 12 months, so, if your child makes it to 12 months and is still in partial-remission, you won the lottery and are doing something right so congratulations!
Vol. 32(8): 1384-1390, Aug 2009
Glostrup University Hospital, Denmark
Dept of Pediatrics, Hannover, Germany
University of Ulm, Germany
University Children's Hospital, Switzerland
How Often Children Achieve Remission
and Partial Remission of Type-1 Diabetes
To determine if and how often remission and partial remission occurred in children, researchers in Kuwait studied 103 recently diagnosed diabeteic children under the age of 12 and followed their conditions for several years. Of the 103 diabetic children unger than 12 years old, partial remission occurred in 71 children and complete remission in 3. Partial remission began in this study about 29 days after diagnosis and continued for an average of 7 months. All children had lost their remission status after 13 months with most ending after 7 months. The honeymoon perdiod was defined as having insulin requirements of less than 0.5 Units per kilogram body weight per day and an A1C of less or equal to 6%.
Vol. 7(2): 101-107, April 2006
Endocrine Unit, Pediatric Dep
Farwaniya Hosspital, Kuwait
Remission & Partial Remission in 242 Diabetic Children
What to expect when your child gets diabetes is the question burning on the mind of every parent. Parents wonder if their child will have it for life? - Are some cured of the disease? - What health consequences to expect, etc. In this study out of Belgiu - 242 children under age 15 were followed after diagnosis of type 1 diabetes. Blood tests were taken at 1 month, 6 months and 12 months to look for changes in glucose and insulin output to see how their conditions progressed. While no children achieved complete remission (where no insulin was needed), 56% of the group did achieve the definition of partial remission (also called the honeymoon period) which lasted 9.2 months on average after diagnosis. Partial remission was defined as having an A1C below 6%. Blood samples also showed a steady decline at each testing period. No children were shown to have improvement of insulin output during the 12 months.
Vol. 2014 (2014)
Pediatric Endocrinology Unit
Univesite' Catholique de Louvain
Brussels, Belgium
Researchers state "Type 1 Can Be Reversed"
Evidence of New Beta Cell Growth
in People with Type-1 Diabetes
Insulin secretion is detectable in some people with long-standing type-1 diabetes, indicating either a small population of surviving beta-cells or continued renewal of beta-cells subject to ongoing autoimmune destruction. In this study, 42 individuals with type-1 diabetes and 14 non-diabeteic individuals were evaluated for presence of beta-cells, beta cell apoptosis (destruction), beta cell replication and T-lymphocytes and macrophages. Results showed 88% of people with type-1 diabetes had active living beta-cells. Beta cell destruction was twice as likely in type-1 diabetes as control subjects. In conclulsion, the researchers stated,
Vol. 48(11):2221-8, October 5, 2005
Larry Hillblom Islet Research Center
UCLA David Gefen School of Medicine
Los Angeles, California
New Beta-Cells Grow in Pancreas by Division of Older Beta-Cells
In principle, new beta-cells can grow from stem cells (as occurs in blood, skin and intestine) or by duplication of existing cells. Giving a brief review of previous studies, the researchers stated new beta-cells are believed to grow from cells lining the pancreatic ducts - from inside the islets - or in bone marrow. Like catepillars to butterflies, other studies suggest that new beta-cells form in adults when cells called acinar cells located in the islets transform into beta-cells. In this current study at Harvard University, researchers found a way to show that the major source of new beta-cells formed in adults (and in pancreas damaged in mice) is from pre-existing beta-cells, rather than stem cells.
CHEM-TOX COMMENT: If this study is correct (that new beta-cells form from existing beta-cells), it suggests the importance of removing autoimmune factors before total destruction occurs to all beta-cells in the pancreas.
Vol. 429: 41-46, May 2004
Dept. of Molecular and Cellular Biology
Howard Hughes Medical Institute
Harvard University
Cambridge, Massachusetts
Yuval Dor, et. al
Remission Can Be Done!
Rare Documentation of Permanent Remission of Type 1 Diabetes
This situation shows a complete and permanent remission of type-1 diabetes is possible. The following provides an example of one patient who had GADA autoantibodies at diagnosis but when tested at 5 and12 years later, the antibodies were no longer present and the patient had reached normal insulin production. Again referring to the original study above of 107 adults diagnosed with diabetes, patients were tested in follow-ups at 3, 5 and 12 years after the orignal diagnosis of diabetes. Follow-up testing showed practically all patients had worse (lower) insulin output (as measured by the c-peptide test) as years progressed. Complete beta-cell failure was present in only 4 of the 107 at diagnosis but was present in 21 patients five years later. It is interesting to mention that while insulin output decreased for nearly all of the 107 patients during the 12 years, two patients did not follow the trend. In fact, these two people were producingto produce normal levels of insulin 5 and 12 years after diagnosis. Of the 5 patients positive for GADA antibodies at time of diagnosis, 4 of these individuals developed complete beta-cell failure at some point during the 12 year study, however, the 5th patient did not. In fact, the 5th patient with GADA antibodies showed significantly improved insulin output from his beta-cells. Three years after diagnosis, his c-peptide levels were 0.55 nmol/l - however, 5 years after diagnosis, he no longer had the GADA antibodies and C-peptide had increased to 1.09. After 12 years his C-Peptide levels were still in the normal range at 1.08 nmol/l.
Vol. 51(6): 1754-62, June 2002
Department of Endocrinology
Lund University
Malmo University Hospital
Malmo, Sweden
"Patients with one antibody at diagnosis" - second paragraph.
Evidence Humans Do in Fact Grow New Beta-Cells but is Highly Affected by Glucose Levels and Age
In the scientific community, it is well known that animals have the ability to regenerate new pancreatic beta-cells, but this also depends on age. For example, while young rats can grow beta-cells at a relatively fast pace (as seen after intentional damage to the pancreas), the rate decreases to about 1-3% per day in older rats. Although beta-cell growth is believed to also occur in humans, the extent of this regeneration is not well understood and can be reduced (or eliminated) if autoimmune cells or high blood glucose levels (called glucose toxicity) destroy immature beta-cells "trying to grow" in the pancreas. To determine if and how well humans can grow new beta-cells, scientists measured the growth (and death) of cultured human beta-cells under different glucose concentrations from 53 organ donors ranging in age from 17 to 74 years. In both older rats and humans, increasing glucose from 100 mg/dl (5.5 mmol/l) to 600 mg/dl (33.3 mmol/l) resulted in a linear increase in beta-cell death and large reduction in proliferation. Age was also a major factor as beta-cells from older donors died in far less time at higher glucose levels.
Vol. 55(9), 2455-2462, Sept 2006
Marc Y. Donath, MD
Division of Endocrinology & Diabetes
Dept. of Medicine
University Hospital
Zurich, Switzerland
Beta-Cells Replenish and Grow in Adult Lewis Rats
As people with type-1 diabetes (and now type 2) have lower numbers of beta-cells in their pancreas, it is important to determine to what extent humans can regenerate lost or damaged beta-cells that produce insulin. Scientists at the University of Barcelona set out to determine how fast beta-cells reproduced - how many beta-cells were destroyed and the beta-cell mass in Lewis rats at different times throughout their lifespan. Lewis rats can often live up to 24 months. They divided rats into different groups and performed humane killings and subsequent pancreas analysis at 1 month - 3 months - 7 months - 10 months - 15 months and 20 months. Results showed beta-cell mass increased 8 times from 1 month to 20 months (typically a very old rat). The number of beta-cells per pancreas also tripled from month 1 to month 7. In their "DISCUSSION" - scientists stated that this is the first study to show that beta-cell growth is maintained throughout the entire lifespan in normal rats and that beta-cell growth remains stable after young adulthood, clearly establishing that beta-cell birth rate does not fall to 0, even in late periods of life.
Vol. 49(8): 1341-1346, Aug 2000
Laboratory of Diabetes & Exp Encocrin
University of Barcelona, Spain
"Magical" Hormone Stimulates Beta-Cell Growth
Since the ability of the pancreas to regenerate new beta-cells is no longer theory and well documented to occur in both children and adults, it would be helpful to identify if anything takes place inside the body that encourages new beta-cell growth. Scientists at the Joslin Research Laboratories in Boston, Massachusetts were able identify one of these processes. What they found is that all of us have a network of specialized cells located in the lining of our intestine. These cells have the ability to produce what might be defined as a "magical" hormone known as "exendin-4." The reason for the word "magical" is that when this hormone is excreted by the intestinal cells - it then enters the blood and the hormone then works as a signal telling other parts of the body to begin growing "new" beta-cells. These new beta-cells then grow from special areas in the pancreas known as progenitor ducts and can also grow from remaining beta-cells in the pancreas. Other research has shown beta-cells can even grow from alpha-cells within the pancreas as well.
When this new beta-cell growth process starts, the body is attempting to replace beta-cells that have been destroyed by autoimmunity. You could almost say there is an ongoing race between one team trying to destroy beta-cells and the another team trying to build beta-cells. Unfortunately for children with type-1 diabetes, the team destroying beta-calls is winning, although the hormone "exendin-4 is trying its best to help the "building team" turn this around.
For the patient in the earlier example who achieved complete remission of diabetes (which continued for more than 10 years after diagnosis) - the autoimmune destroyer team didn't win that race, in this situation, the beta-cell building team was the winner since it was able to grow back beta-cells faster than they were being destroyed. All of this was apparently successful because of something that person did or something that changed in that person's life (either knowingly or unknowingly).
Vol. 48(12): 2270-2276, Dec 1999
Exercise Prevents Damage From High Sugar Diet
While a person with a healthy pancreas rarely has blood sugar numbers over 120 (no matter what they eat), a person with prediabetes can easily reach blood sugar levels of 160, 180 or even 200 after a normal meal. Throw in cake and ice cream at their next birthday party and it could hit 250 one hour after eating. Since having sugar levels this high has been shown to damage insulin production in beta-cells in the pancreas (and thereby accelerate the appearance of diabetes), it would certainly be helpful to find some way to prevent or at least quickly reduce blood sugar levels in a prediabetic (or diabetic person suffering an episode of insulin resistance), for example, after a birthday party or a moment of weakness strolling down the cookie isle at the grocery store. The good news, apparently there is something that can be done that can help keep blood sugars more normal, even if eating more than what is considered healthy.
Researchers in at the University Federal de Ouro in Brazil took 96 rats (known as Wistar rats) and divided them into four groups. Group 1 ate standard chow and relaxed on the couch as much as they wanted. Group 2 also ate standard chow but was forced to swim 5 days a week for up to an hour. Group 3 was fed a high sugar diet and was a couch potato as well. Group 4 ate a high sugar diet but was also forced to 5 swimming periods weekly.
After "training," the animals were sacrificed and samples taken of fat cells and skeletal muscle. Results showed that rats receiving exercise had greatly increased density of mitochondria. Since mitochondria provide energy for cell function, this demonstrates that exercise can greatly improve metabolic function in the animals. Of great importance, it was found that rats given the high sugar diet had less damage to their cell structures and less inslulin resistance if they engaged in exercise. In conclusion the researchers stated,

